Our environment and in particular the workplace, is at the heart of the increasing incidence of cancer.
An occuptional cancer is the result of a worker’s exposure to a cancer-causing agent in the workplace.
Useful to know
Exposure can come from various sources:
- Airborne (dust, fumes, mists)
- Ingestion of particles that have come into contact with lips or hands,
- skin contact.
The more frequent and prolonged the exposure, the greater the risk. But even limited exposure can cause cancer.
Occupational cancers generally appear 10-50 years after exposure to the cancer-causing agent (latency period).
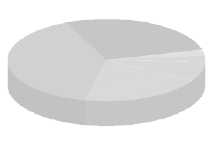
The figures
- 11,000 - 23,000 new cases of cancer annually
- 2.3 million people are exposed to carcinogens
- 70 % of those exposed are manual workers
- 1 in 5 cancers amongst manual workers is work-related
- 90 % of occupational cancers are linked to asbestos.
Occupational cancers generally appear 10-50 years after exposure to the cancer-causing agent (latency period).
Substances responsible
Agents causing occupational cancers are numerous and in widespread use in the workplace :Asbestos is now banned in France. Benzene, vinyl chloride, silica, lead and sawdust, these cancer-causing agents all have workplace exposure limits [valeurs limites d’exposition professionnelle (VLEP)]. All the others can only be used in restricted circumstances in the workplace.
There are various classifications of cancer-causing agents including those of the European Union which stipulate labelling requirements, and those of the International Agency for Research on Cancer (CIRC/IARC), which are based on scientific consensus and which evolve as knowledge develops.
- Chemicals:
benzene, tars, mineral oils, mineral fibres, sawdust etc. - Physical agents :
onising and ultraviolet radiation - Biological agents :
including hepatitis B and C
Know what you are using
Consulter l’étiquette qui figure sur le produit que vous utilisez.
Pas d’étiquette ? Une étiquette qui semble anodine ? Renseignez-vous impérativement avant de manipuler le produit car il a pu être transvasé d’un autre récipient.
En savoir plus : www.inrs.fr
Get hold of the safety notice
Every substance must be provided with a safety notice containing health and safety advice. It must be made available to users. However it may be incomplete and, worse, misleading by providing over-generalized descriptions.
![]() If you see this symbol, it means the substance can cause cancer.
If you see this symbol, it means the substance can cause cancer.

Your employer has obligations.
Your employer must:

Carry out regular risk assessments (work done, substances used, length of exposure etc) taking account of actual working conditions and any incidents reported. The employer must create a “central evaluation document” [document unique d’évaluation] for risks which sets out the safety measures to be employed;
Replace dangerous substances by safe or less dangerous substances :
www.substitution-cmr.fr
Reduce exposure to the minimum: reduce exposure periods and the number of employees so exposed.
Provide any employee exposed to a carcinogen with written information and refresher training stressing the health risks, precautions to take, procedures to follow, the wearing and upkeep of personal protective equipment.

Provide personal protective equipment
You’ve got rights
 Are you exposed to cancer-causing agents?
Are you exposed to cancer-causing agents?
- You are entitled to additional medical supervision: Medical checkups must be at least annual, except for night-shift workers for whom they must be 6 monthly;
- our employer must retain your medical file for 50 years following exposure. It can be supplied to you on request.
- A certificate of exposure [attestation d’exposition] must be provided when you leave your employment, whatever the reason for departure.
- The occupational health doctor must offer you post-employment follow-up (for retirement, unemployment, changing jobs)
 Have you been exposed to cancer-causing agents?
Have you been exposed to cancer-causing agents?
If you suffered exposure and are unemployed, looking for work or retired, your are entitled to a free medical checkup every 2 years. This checkup involves regular, specific examinations thus allowing early detection of cancer, making treatment more effective. You can request this checkup from your medical insurance provider
NB If you don’t have the certificate of exposure from your employer and the occupational health doctor, your insurer [caisse] will have to check that you suffered exposure in the past.
Under what circumstances can you claim compensation ?
For anyone suffering from a work-related cancer it is vital that it be recognised as such for you to have your medical costs fully covered.
Depending on the cancer, there are two ways of getting it’s work-related nature recognised :

If the cancer is listed in an occupational injury register [tableau de maladie professionnelle]
Any case meeting the conditions of a register is automatically presumed to be occupational and requires no proof. Each register contains a list of diseases (medical certificates must use the terminology of the table) a restricted or general list of occupations and a deadline for assuming responsibility (maximum amount of time since the end of the exposure).
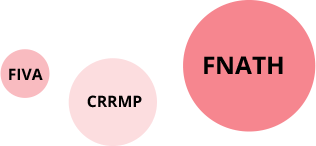
If the cancer is listed in a register but the conditions listed in the register are not entirely satisfied or where there is no register, the occupational nature of the cancer is decided by the regional committee for recognising occupational diseases [Comité Régional de Reconnaissance des Maladies Professionnelles (CRRMP)].
For asbestos-related cancers, compensation may be available through the compensation fund for victims of asbestos [Fonds d'Indemnisation des victimes de l'Amiante (FIVA)] : www.fiva.fr
What is FNATH ?
FNATH, the association for occupational accidents, has been supporting victims of occupational injuries (accidents at work or occupational diseases) since 1921.
Through its large country-wide network of legal and medical experts, FNATH advises and supports victims of accidents.